Scientists are developing a robotic sleeve that can encase a flabby diseased heart and gently squeeze to keep it pumping.
So far it’s been tested only in animals, improving blood flow in pigs. But this “soft robotic” device mimics the natural movements of a beating heart, a strategy for next-generation treatments of deadly heart failure.
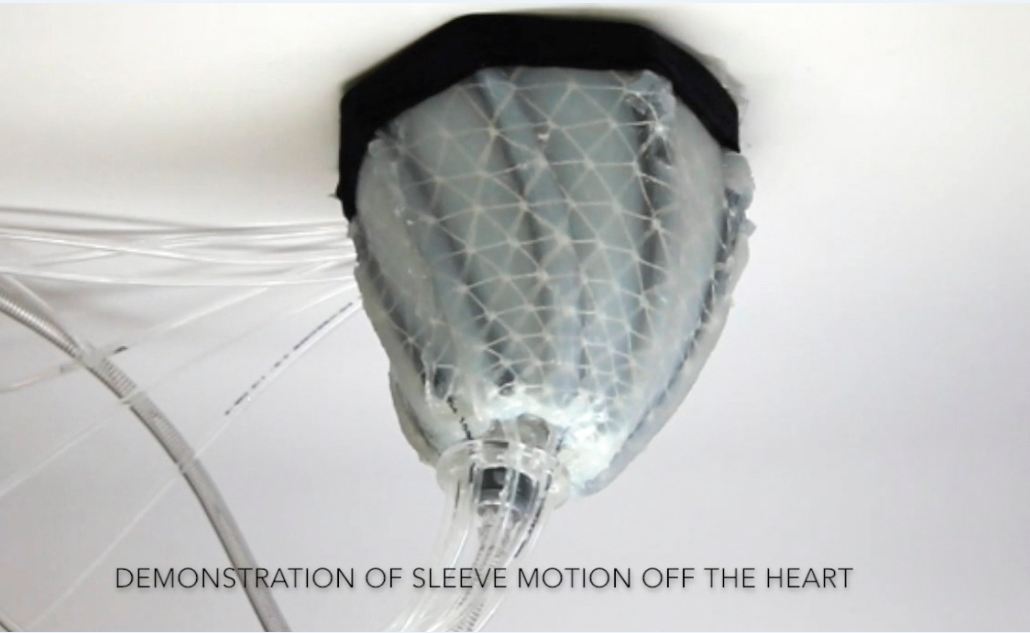
The key: A team from Harvard University and Boston Children’s Hospital wound artificial muscles into the thin silicone sleeve, so that it alternately compresses, twists and relaxes in synchrony with the heart tissue underneath.
It’s a dramatically different approach than today’s therapies and, if it eventually is proven in people, it might offer a new alternative to heart transplants or maybe even aid in recovery.
“You can customize the function of the assist device to meet the individual needs of that heart,” said Dr. Frank Pigula, a cardiac surgeon who, while at Boston Children’s, took the idea to Harvard colleagues developing soft robotics.
More than 5 million Americans, and 41 million people worldwide, suffer heart failure, a number growing as the population ages. A heart left damaged by a heart attack, high blood pressure or other conditions becomes progressively weaker and unable to pump properly.
For severe cases, the only options are a scarce heart transplant or battery-powered mechanical pumps that are implanted into the chest to take over the job of pumping blood. These VADs, ventricular assist devices, prolong life, but running blood through the machinery can leave patients at risk of blood clots, strokes and bleeding.
That shouldn’t be a risk with the robotic sleeve.
“The nice thing about this is it can go on the outside of the heart, so it doesn’t have to contact blood at all,” said Harvard associate engineering professor Conor Walsh, senior author of the research published Wednesday.
Unlike with traditional rigid medical devices, the soft robotics approach allowed design of a sleeve that could fit snugly over a heart’s irregular surfaces. It moves thanks to artificial muscles, a concept developed in the polio era that’s now being used in robotics. They’re powered by pressurized air that would have to be carried in a pump in a backpack or fanny pack much like the batteries that power today’s VADs.
The researchers programmed the robotic sleeve to move in the same pattern as the weakened heart muscle it surrounds while strengthening and optimizing each heartbeat. The device can be tailored to compress different sections of the heart.
And importantly, as the sleeve relaxes, it helps the damaged heart better expand and refill with blood ready to be pumped out with the next heartbeat, said Pigula, who is now with the University of Louisville.
The big test: The sleeve restored normal blood flow in six pigs that had been put into heart failure, Walsh’s team reported in the journal Science Translational Medicine.
The experiments were short, lasting only a few hours, and more research to test how long animals could live safely with the implanted sleeve is crucial before it ever could be studied in people, Walsh cautioned. He’d also like to study if physically moving damaged heart muscle — essentially exercising it — might spur it to heal and require less assistance from the sleeve over time.
“I’m quite impressed with where this research is going,” said Dr. Christopher O’Connor, chief executive of the Inova Heart and Vascular Institute in suburban Washington, who wasn’t involved with the sleeve’s development.
Researchers have previously tried “socks” and other ways to encase or compress the heart with little success.
Unlike those prior attempts, the new sleeve is “smart, it’s robotic,” said O’Connor, who edits an American College of Cardiology heart failure journal. “They really worked on developing a device that can mimic the contraction of the weakened heart muscle and augment it so there is improved heart function without the theoretical clot risk.”—AP
Image: AP